The Inflamed Mind
Inflammation is linked to obesity, diabetes and depression, but its full action and impact are only just beginning to be understood
Professor Ed Bullmore is a psychiatrist and neuroscientist who thinks more deeply than most about the state of his teeth. In his 2018 book, The Inflamed Mind, Bullmore chews over a particularly painful chapter in his dental history: an old filling had become rotten and infected and required root-canal surgery. “As soon as it was all done, I wanted to go home, go to bed and not talk to anyone,” Bullmore recalls. “And when I was alone at home I found myself cogitating gloomily on the grave until I went to sleep.”
In time, that experience would prove pivotal. For part of his career, Bullmore worked closely with GlaxoSmithKline. The pharmaceutical firm was an active player in the search for new drugs against depression, but in 2010 it exited the field. Despite deep pockets and talented staff, the industry had failed to find better treatments for depression – so Bullmore decided to drill down into the roots of that failure. “One key reason was that all the failed trials assumed that depression is one thing and that there will be a panacea that works for everybody,” he says. “I think that flies in the face of common sense and emerging science.”
Some of the emerging science Bullmore started looking at involved immunology, a field he had last studied at medical school two decades earlier, and what he discovered amazed him. “When I looked at modern textbooks it was like a palimpsest: I could see through the diagrams to the crude version that I’d been taught, yet overlaid was this huge amount of detail. And not just detail. Many of the big things we were taught as students – like the Berlin Wall of the blood-brain barrier – were wrong.”
Bullmore cast his mind back to the gloom he had experienced and began to wonder whether the inflammatory response could have caused his low mood. The more he read, the more it made sense
Bullmore cast his mind back to the existential gloom he had experienced after his root-canal treatment and began to wonder whether the inflammatory response his immune system had mounted against his infected tooth could have caused his low mood. The more he read, the more it made sense. Take cytokines, for example, the inflammatory proteins pumped out by macrophages into our immune system in response to injury or infection. If you inject them into rats, they become sleepy and sluggish, and stop taking pleasure from the sugar water they normally enjoy. If you treat hepatitis patients with interferon – a drug that gives the immune system a massive boost – one-third will develop clinical depression six weeks later. And a large-scale, long-term study revealed that increased levels of cytokines in the blood of nine-year-old children were strongly linked to the development of depression at age 18.
Given mounting evidence that inflammation can cause depression, and the fact that it is both common and costly (one in four of us will develop depression at some point in our lives, and it is set to be the biggest single cause of disability by 2030), Bullmore believes that viewing it as an inflammatory syndrome could lead to new ways of diagnosing and treating some forms of the illness. “There are still some important questions to resolve,” he says, “like whether or not targeting inflammation can make a difference to treatment; we’ve not yet seen convincing data from a trial designed to test that idea.”
The common thread
Bullmore’s new trial, launched in September 2019, could provide an answer. The trial is planning to recruit 1,420 patients from Glasgow, Cardiff, Oxford and London as well as Cambridge, whose depression has not responded to SSRIs (the current frontline antidepressant drug treatment). Half will receive a P2X7 antagonist – a drug that stops stress signals triggering an inflammatory response by the immune cells in the brain. “The P2X7 receptor is a critical step on the path from stress to inflammation, so we hope that by giving people this drug, we can protect stressed people from also becoming inflamed – and that might make them less depressed,” he says.
However, depression is only one of many increasingly common diseases – from diabetes and dementia, to cancer and heart disease – that scientists now think could be caused by inflammation. At the Wellcome-MRC Institute of Metabolic Science, Professor Antonio Vidal-Puig is unpicking the molecular mechanisms that link obesity with insulin resistance, diabetes and heart disease in order to find new forms of treatment.
Obesity is associated with diseases like Alzheimer’s, autoimmune and other common diseases – we think inflammation is the common thread that links them all
“The big question we’re trying to address is why people who are obese develop metabolic complications like diabetes and cardiovascular disease,” he says. “Obesity is also associated with neurodegenerative diseases like Alzheimer’s, autoimmune diseases and many other common diseases, and we think inflammation is the common thread that links them all.”
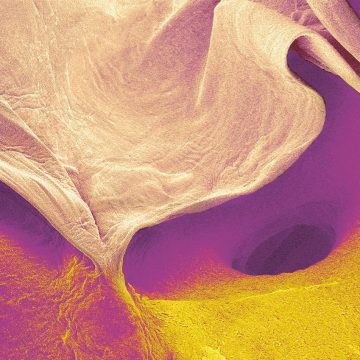
Vidal-Puig and his group are interested in why obesity sets off this inflammatory chain of events. Their work revolves around an idea they call “adipose tissue expandability”, a simple yet radical idea that our fat cells or adipocytes have a finite capacity for storing fat and that things go awry once this capacity is breached.
“When you see someone in the obesity clinic who is 190kg [30st], it’s easy to get the impression that adipose tissue can go on forever, but we now have data suggesting that genetic factors may uncouple obesity from metabolic complications. Some obese people are healthy – they have no diabetes or heart disease – and some very lean people are sick,” he explains. “Where we once thought people got sick because they were obese, we now think it’s because their fat stores are full. It’s like looking at the same picture but arriving at two different explanations – and that has different implications.”
Flame and the detonation
Part of the idea stems from how macrophages respond to fat. When adipocytes become full and start leaking fat, it is the macrophages that mop things up. And when those macrophages become full of fat they behave as if they’re fighting an infection, pumping out cytokines into the immune system. “The macrophages are confused,” says Vidal-Puig, “possibly because they misinterpret the fat from adipocytes as the lipids found in the cell wall of bacteria, so the lipids from our food are somehow triggering responses that are abnormal.”
His key aims now are to gain a deeper understanding of how adipose tissue works, how we can best get rid of excess lipids, and which types of lipid are the most inflammatory. He hopes it will then be possible to stop the inflammation before it starts. “Dealing with inflammation is too late, because it’s like a bomb. When a bomb explodes it splits into more fragments than you can possibly deal with. So we want to act before the bomb goes off – to try to prevent the flame that causes the detonation.”
It’s the classic ‘looking under the lamp-post for your lost keys’. Everybody looks where the light is, but that doesn’t mean it’s where you’ll find your keys.
This rationale is also behind a huge new effort to understand and treat cancers differently, and, in 2019, Cancer Research UK (CRUK) announced a £20m Grand Challenge award involving an international team of scientists from the US, Canada, the UK and Israel to find new ways of tackling cancers linked to chronic inflammation.
Globally, around 20-25 per cent of cancers are linked to chronic inflammation, including oesophageal, bowel and pancreatic cancer. Incidence of these cancers is rising, and while 57 per cent of the 42,000 people in the UK diagnosed with bowel cancer between 2014 and 2016 will survive, the outlook for others is much poorer. For oesophageal cancer, 9,101 cases were diagnosed during the same period and the 10-year survival rate is 12 per cent while 59 per cent of oesophageal cancers are preventable.
Holistic
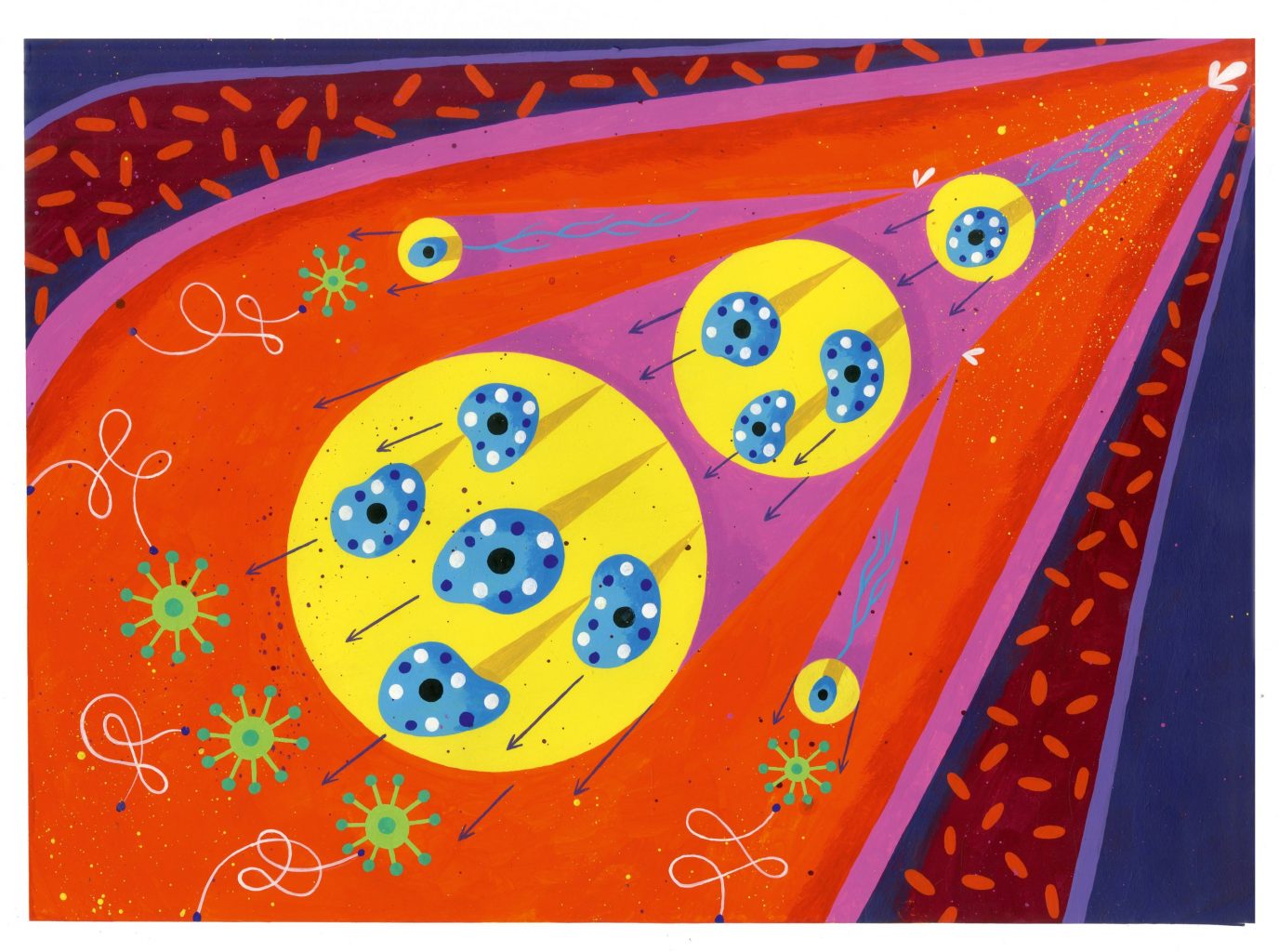
Dr Doug Winton of the CRUK Cambridge Institute is part of Grand Challenge. He believes that it is time to take a fresh look at these kinds of cancer. “A large part of the Grand Challenge is about pushing back against the idea of epithelial cancers arising just due to cancer-driving mutations. “It’s about thinking in a more holistic way,” he says. “The epithelium is only one cell type among a community of cell types. They all interact, regulate and monitor each other, and our tissues are communities of cells that all relate to each other.”
Inflammation is involved in nearly all cancers, not least because cancer usually causes inflammation – but for some cancers it is the inflammation that causes the disease. And while this idea is not new, what has changed is our ability to study communities of cells in minute detail. “It’s the classic ‘looking under the lamp-post for your lost keys’,” says Winton. “Everybody looks where the light is, but that doesn’t mean it’s where you’ll find your keys.”
The Grand Challenge will be using two clever sources of illumination, called CODEX and Organs-on-Chips. Developed by Professor Garry Nolan at Stanford University in the US, CODEX employs myriad markers that allow researchers to identify and map all the cell types present in a tissue, and to do so dynamically as the tissue changes. Organs-on-Chips – developed by Harvard University’s Wyss Institute – is a way of studying tissues outside the body by taking cells of interest and growing them on a chip supplied with a pseudo blood supply.
He began to wonder whether the inflammatory response his immune system had mounted against his infected tooth could have caused his low mood.
Taking cells from oesophageal cancer patients in Montreal, Canada, at different stages of the disease, the new tools will allow the team to build up a detailed picture of how communities of cells behave as the disease progresses.
“Oesophageal cancer is the poster child for this project because it begins with a normal epithelium, which changes to become metaplastic, dysplastic and then cancerous,” Dr Doug Winton, CRUK Cambridge Institute, explains. “Something causes inflammation, such as acid reflux, and the normal epithelium tries to protect itself by becoming metaplastic. This tissue looks like something further down the gut, where the environment is much more hostile. This tissue then becomes dysplastic, or more disordered, and it is this that can develop into cancer.”
By getting a more complete picture of all the players in this process, Winton and the team should be in a better position to change the course of the disease – predicting which patients go on to develop cancer, and how these cellular changes can be halted and repaired earlier. Because by using new tools and ideas instead of looking under the same old lamp-post, we stand a better chance of finding new ways to combat cancer, depression, diabetes and dementia.
Learn more about Professor Bullmore’s new trial.