NHS at 75
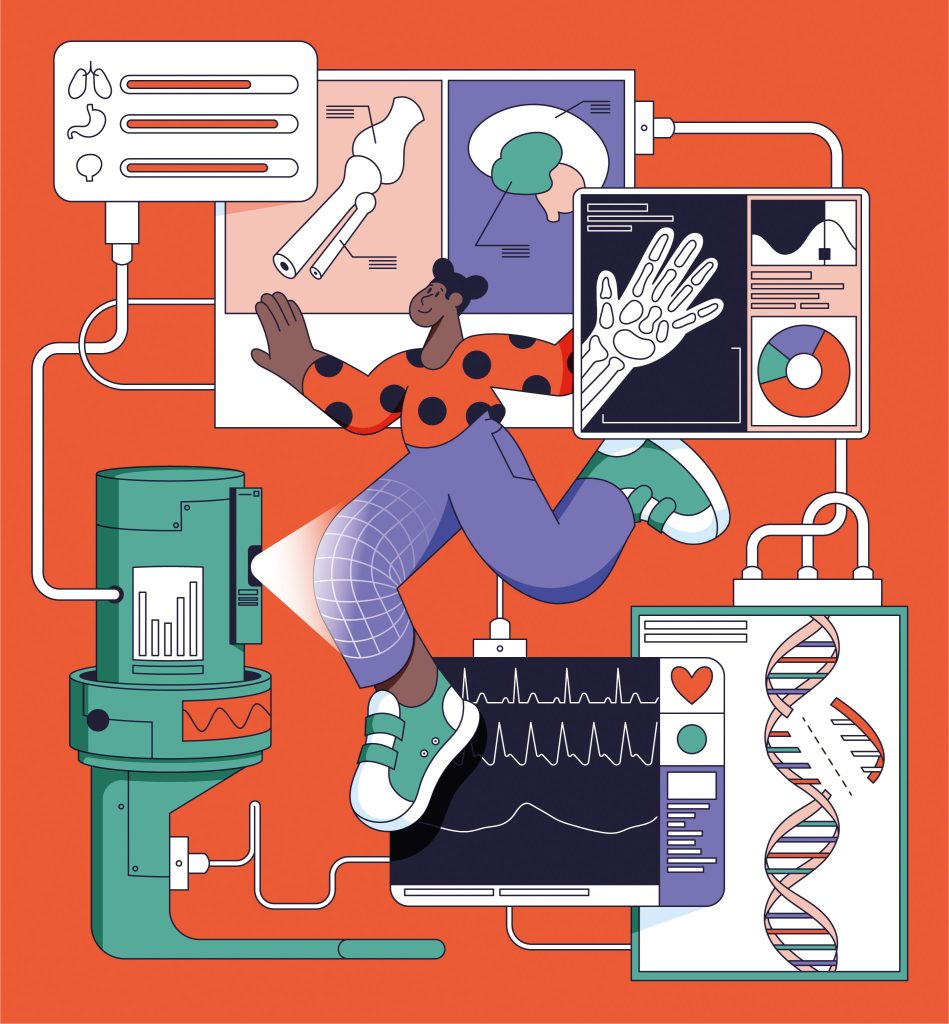
The NHS treats more than a million patients a day but, at 75 years old, it’s never been under more pressure. So, is it still fit for purpose? And what will the next 75 years bring?
This summer, the NHS celebrated its 75th birthday with strikes, a lack of beds, concerns about care quality and outcomes, and low workforce morale. Meanwhile, arguments raged about the solutions: more money, more people, more tech, more prevention, more external collaboration? Whatever that future looks like, the time to build it is now – because the NHS’s life is in our hands.
But given where we are, can the NHS be fixed? Where do we start? How do we decide what we’re going to fix – and when? We asked Cambridge experts for their prescription on what’s next for our beloved healthcare system.
Get early detection right
The fixes could start the moment a child is born. Early detection, says Professor Richard Gilbertson, Li Ka Shing Chair of Oncology, has the capacity to transform the way we treat all diseases. “As our population ages and grows, everyone ending up in hospital is not sustainable. It’s a failed, expensive system and as it gets more and more expensive, sooner or later, we won’t be able to pay for it.” Gilbertson argues that patients who go to hospital in the late stages of their disease tend to have worse outcomes, as well as being more expensive to treat. So the new Cambridge Cancer Research Hospital is designed around the principle of identifying potential health problems as soon as they arise. The UK is a world leader in this field, with projects such as UK Biobank – a large-scale biomedical database and research resource, containing in-depth genetic and health information from half a million UK participants. “These projects are beginning to help us understand what a patient’s disease risk is from an early age – and how we can manage that, with programmes including diet, exercise and risk management.”
Researchers are developing increasingly accurate and sensitive ways of picking up disease even earlier. The question, says Gilbertson, is how we implement and identify biomarkers that cover a multitude of diseases. “For example, everyone knows that if you smoke, you’re at risk of lung cancer – but you’re also at risk of heart disease, stroke and peripheral vascular disease. We know that there are genetic factors and other environmental factors which also put us at risk of certain diseases. So now we’re not just talking about screening, but holistic healthcare pathways that consider all those factors.
Let’s get physicists, chemists, engineers and mathematicians designing these new early detection systems with primary care doctors who know what it’s like to work in high streets across the UK
“If we were to think about that in a systemised way, alongside those big data opportunities, we could identify patients in the early stages of cancer, for example, eight or nine years before those symptoms present. That means patients can be treated earlier, closer to home, and more cheaply – and that becomes a sustainable system.”
But to achieve this, we need a cultural shift in the way we train our medical professionals, he believes. “We train people to be experts in how to treat diseases like cardiology, cancer or diabetes. But we need to start thinking about training experts in sustaining health, armed with big data information that can guide new pathways that maintain tissues in a healthy state.
“This will need a change of mindset in the way we think about health and disease and the way the government thinks about health care provision. We will need new pathways that unify primary and tertiary care systems for the future; bringing together physicists, chemists, engineers and mathematicians to design early detection systems with primary care doctors who know what it’s like to work in high streets across the UK.”

Research is for everyone
And all those people deserve equal access to one of the key drivers of improved health: research. Right now, that’s not happening, says Professor David Rowitch, Head of Paediatrics and co-leading for University of Cambridge in the new Cambridge Children’s Hospital.
“If your research does not enable access to the most deprived populations, then we are failing in our mission.”
“The NHS covers 100 per cent of the population, but 25 per cent or more are deprived – people who have the worst physical and mental health outcomes and premature death. If your research does not enable access to the most deprived populations, then we are failing in our mission.”
Part of the solution lies in future hospital design, he says: building all hospitals to support regional research capacity, for example, places to talk to research participants, specific types of diagnostic equipment, and specimen collection stations in district hospitals and the community.
Still, the national organisation of the NHS – as opposed to a fragmentary, competitive system such as that found in the US – means that it has a much greater ability to scale rapidly. He points to the nationwide RECOVERY trial that discovered the benefits of dexamethasone to treat severe Covid-19 as an example.
Rowitch adds that while Covid research demonstrated a response to a national crisis, it is also possible for new regional hospitals to level up research opportunities as routine. “It may be more efficient and compelling to look at the needs in a region, especially areas of deprivation, and organise our research to address causes of disease before escalation to hospital.”
Co-designed solutions are best
Having this truly national health service enables outcomes to be tracked, measured and compared centrally. Data plays a big part in this – and will play a far bigger one in the next 75 years. But while data tells you what the problem is, people working together will tell you how to solve it, says Mary Dixon-Woods, Director of The Healthcare Improvement Studies (THIS) Institute and the Health Foundation Professor of Healthcare Improvement Studies.
“Data allows the NHS to track not just outcomes, but processes,” she says. “Outcomes are what happens as a result of your treatment; you have an operation and make a good recovery. Processes are what you do to get to that outcome – everything from prescribing to culture to behaviour. So we need good evidence about what you need to do in order to improve those processes.”
Top-down improvement efforts have a poor track record.
Top-down improvement efforts have a poor track record. New processes may not be well designed or feel imposed, and staff asked to carry them out may be alienated by them, she points out. But bottom-up may not be the answer either. Leaving it up to people to work out process by themselves can also be challenging, because they don’t always have access to resources, expertise and time.
That’s why, says Dixon-Woods, the future of the NHS lies in co-design – enabling patients and staff to design a solution together. When the pandemic started, hundreds of different clinical processes needed adaptation. “If everyone comes up with their own method, they might not have the expertise or capacity, and it’s potentially wasteful and time-wasting,” she explains. “For example, when someone experiences a postpartum haemorrhage – a massive bleed after giving birth – there is a very clear set of tasks. Do them right and on time and you usually have a very good outcome. But we had to change the processes to consider what to do when the person might be Covid positive.”
Using the Thiscovery platform, Dixon-Woods’ team created a short video that illustrated possible processes, bringing together maternity staff, infection control experts and human factor experts, who specialise in system design. Using online consensus-building techniques, 16 improvements were identified – the video illustrates the improved processes and has had more than 130,000 downloads on YouTube.
“I’m hopeful that the NHS as a whole will see the huge benefits in essentially standardising practice through genuine co-design with staff and patients,” says Dixon-Woods. “A non-hierarchical system for process improvement is more inclusive – but more importantly, it’s much more likely to get you to a good place, both in terms of outcomes and in terms of cost, by stripping out the waste of everyone doing things differently. The NHS is fantastic people doing fantastic things; they just need facilitation and support.”
Time to change
This co-design relies on people, and finding – and keeping – those people is the biggest challenge the health services face right now. “We don’t have enough people to do everything that the NHS is currently tasked to do,” says Charlotte Summers, Professor of Intensive Care Medicine and Director of Cambridge’s new Victor Phillip Dahdaleh Heart & Lung Research Institute. “We can recruit and train more people, but we must also retain the ones we’ve got. Right now, the nursing resignation rate is the highest it’s ever been. We’ve got to find a way to make the NHS a better place to work.”
Intensive care doesn’t just need trained specialist nurses but occupational therapists, speech and language therapists, physiotherapists, pharmacists and administrators, she says. “And right now, there are holes in every bit of that workforce.”
“Any governments of the future must engage with the NHS meaningfully.”
Summers says that when services are cut to the bone, all the extra bits that make your job satisfying and enjoyable – such as training, support, research and even the ability to afford the basics of life – get squeezed. “Nurses are being forced to use food banks. Junior doctors are not able to afford childcare to look after their children, because they’re rotating three hours away to a hospital at six weeks’ notice. People do not stay with employers under these circumstances.” And the argument that the NHS spends too much on managers? “Research shows that, if anything, the NHS is under-managed,” says Summers. “Managers are a necessary part of any complex organisation. Who is going to manage the supply chain that ensures my patients have the oxygen they need?”
Summers is clear that she is not proposing another reorganisation: these have a long history of disruption and damage. “But the frameworks are in place to do what I think is needed – a cultural change and a mindset change.” As the NHS workforce looks to the next 75 years, she says it’s time for government to think differently, too. “Any governments of the future must engage with the NHS meaningfully. They must support and nurture it, rather than saying it’s just too difficult. It’s a choice to decide that it’s too hard.”
-
Changing the cancer story
The Cambridge Cancer Research Hospital will change the story of cancer. We will detect cancer earlier, treat it more precisely and save more lives. What happens here in Cambridge will have a huge impact across the region, the UK and the world. The breakthroughs and innovations we deliver will change the way we detect and treat cancer far beyond our hospital, bringing hope to millions of people.
To find out how you can support the work of the Cambridge Cancer Research Hospital, Cambridge Children’s Hospital, the Victor Phillip Dahdaleh Heart & Lung Research Institute or THIS Institute, contact Mary Jane Boland at maryjane.boland@admin.cam.ac.uk