Cytosponging
“A bottle brush for the oesophagus” – Professor Rebecca Fitzgerald’s simple yet ingenious invention is set to transform cancer care.
My mind rebels at stagnation,” says Rebecca Fitzgerald’s literary hero, Sherlock Holmes, in The Sign of Four. “Give me problems, give me work, give me the most abstruse cryptogram, or the most intricate analysis, and I am in my own proper atmosphere.” Fitzgerald loves Holmes, she says, for the same reasons she loves her chosen field of early cancer detection. Both appreciate the human devastation that fiendish problems can leave in their wake, but both know the joy of tackling and solving those problems.
If people are diagnosed too late, it doesn’t matter how good our medicines are
“As a junior doctor, I spent some time working with ovarian cancer patients,” she says. “We had a whole series of young women patients who died, and it made a big impact on me. When people were diagnosed too late, it just didn’t matter how good our medicines were.”
It was as a junior doctor, too, that she first heard about Barrett’s oesophagus, a pre-cancerous condition that can lead to oesophageal cancer (the sixth most common cause of cancer death in the UK). Not everyone with Barrett’s oesophagus goes on to develop cancer, but diagnosing the condition and monitoring its progress results in very early cancer diagnosis. This early diagnosis dramatically increases cancer survival rates.
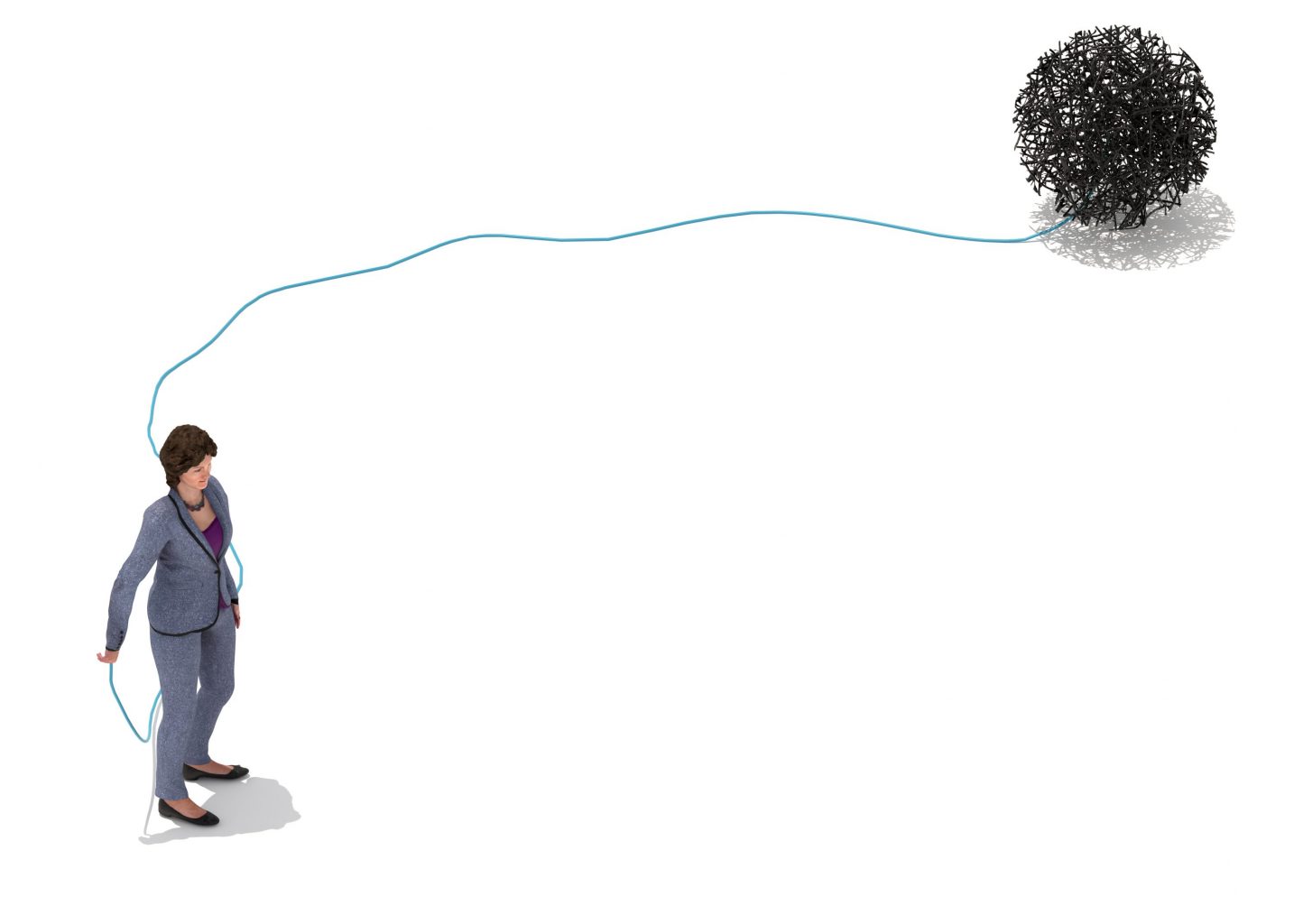
Fitzgerald found this knowledge intriguing: that a pre-cancerous condition existed which could be diagnosed and monitored. But she also found it frustrating. “You knew someone was susceptible. Then you monitored the condition until it was inevitable that the person would get cancer. Then you would treat the cancer. It wasn’t very proactive. I thought that with some problem-solving we could do better.”
Having trained at Cambridge as a gastroenterologist, she initially didn’t think of herself as a researcher. But when her husband’s career took them to Stanford, she found herself unable to practice – so she decided to pursue research. Looking to combine gastroenterology and cancer in a research project, she met George Triadafilopoulos, clinical professor of medicine at Stanford, who specialises in Barrett’s oesophagus.

Barrett’s oesophagus is a condition in which the normal cells that line the oesophagus (the gullet) are replaced with abnormal cells. The main risk factor for the condition is when low pH levels from the stomach move up into the oesophagus, causing chronic reflux. But there was little known about how the acids created by reflux could cause cancer. The pair discussed whether Fitzgerald might be interested in investigating this question. Initially, Fitzgerald’s research found the opposite result from what she was expecting. If she exposed cells to acid, they actually stopped dividing, which looked as if it would prevent rather than cause cancer. “So, then I had a bit of a eureka moment. I realised that the paradigm was wrong. We shouldn’t be exposing the cells to continuous acid: it should be pulsatile, in short bursts, to mimic the reflux. Once we did that, we found that the cells were indeed dividing abnormally. I get most excited about research when I can see the direct relationship to patient care, and this finding meant we could start thinking about the most effective drugs for acid reflux that would keep the acid down and suppress this pulsatile phenomenon.”
Keen to combine research with a range of patient care, she returned to the UK to complete her training at the Department of Adult and Paediatric Gastroenterology at St Barts and the Royal London School of Medicine and Dentistry, working with Professor Michael Farthing, then head of the Digestive Diseases Research Centre. It was a chance discussion with him that led her to the invention for which she is best known: the Cytosponge.
“We were discussing the challenge of collecting samples from patients. I wanted to do continuous monitoring of patients to try to find out what converted benign Barrett’s to cancerous Barrett’s. But monitoring, itself, was a challenge. Doing repeated endoscopies – where you are sedated and a camera on a flexible tube is passed down your throat – is invasive, involved and expensive. Michael said to me: ‘What you really need is a bottle brush for the oesophagus.’”
A pill on a string
Fitzgerald didn’t forget that idea. It stayed with her over the next few busy years, as she completed her training and had her two eldest children. And when she took up a position at the Medical Research Council Cancer Unit in Cambridge, she decided the time had come to investigate it. What if she could create something to quickly identify patients with Barrett’s oesophagus – something that could be more easily swallowed and removed to take frequent and accurate samples from the gullet? “I’m inspired by practical things,” she says. “My husband is an engineer. So, I talked to him and actually had the first Cytosponge prototype made in the engineering workshop.”
It’s a devastatingly simple idea: a pill on a string which expands into a small sponge
It wasn’t perfect: the catheter was too rigid and the end was too sharp. But it was a start. Fitzgerald researched ideas from Japan and China, which both have high rates of oesophageal cancer, and found devices that involved balloons that the patient swallows deflated, and which are then inflated and wiggled around to collect cells before being withdrawn. Balloons didn’t collect many cells, but the inflation/deflation mechanism was promising. Perhaps she needed a material that started off small and could expand? Something, perhaps, like a sponge?
Working with the Medical Research Council and a clinical devices company, she came up with the Cytosponge, which won her the prestigious Westminster Medal. It’s a devastatingly simple idea: a pill on a string, that, when swallowed, expands into a small, rough-textured sponge. When the sponge is pulled back up, it collects cells from the gullet.
But solving the problem needed more than a device for collecting the cells: Fitzgerald and her team needed an accurate and fast diagnostic test. Her team identified a protein which was present in the abnormal cells, and an antibody that could be applied to the cells. This test, known as the Cytosponge-TFF3 test (after the antibody, named Trefoil Factor 3) stains cells brown, allowing them to be easily identified, a process that has now been made quicker using artificial intelligence.
Fitzgerald hoped her method of diagnosing Barrett’s would be at least three times more efficient than the standard GP diagnostic route, which usually involved referring patients for an endoscopy and someone looking down a microscope at tiny biopsies taken from this procedure – a process that was both labour-intensive and prone to error. The most recent Cancer Research UK-funded trial shows that the test is in fact 10 times more efficient. It doesn’t just identify Barrett’s: it is also better at picking up early-stage oesophageal cancer. And the procedure can be performed at a GP surgery by a trained nurse. The extraordinary story of how Fitzgerald created the Cytosponge might seem to have a Conan Doyle-esque simplicity. A problem is identified, investigated and solved, using expertise and ingenuity. But developing a medical device is a far more complex narrative. That original proof of concept work that won Fitzgerald the Westminster Medal was back in 2004. Sixteen years later, the Cytosponge’s rollout across the UK is only just starting.
“To get the data you need around safety, acceptability and efficiency for a device, you need big trials,” Fitzgerald points out. “With a drug, you can often start off with quite small groups to get proof of concept. A device that is going to be used widely has to be acceptable to people who aren’t used to frequent medical intervention. So acceptability is a major stumbling block in early cancer detection and prevention; this explains why it’s been slow to progress compared with drug therapy.
A new era in cancer detection
But the Cytosponge’s success is helping that process to speed up: it’s demonstrated just how important it is to encourage innovation in early cancer detection. The new Cambridge Cancer Research Hospital, for example, will house engineering and physics workshops, prototyping facilities and biology labs that will host experts from all over the world – a natural development from the engineering workshop where the Cytosponge was born. As the Cambridge lead for the International Alliance for Cancer Early Detection (ACED), Fitzgerald is already a champion of such collaborations, which have the potential to transform cancer detection worldwide.
“Someone said to me a year or two ago that it may not, ultimately, be my solution that makes a difference to the diagnostics, but that the idea takes us beyond endoscopy and into a new era,” says Fitzgerald. “And that’s what matters in the end. It’s not about your own individual success. It’s about contributing to the field in a way that has long-lasting effects.”
Rebecca Fitzgerald is Interim Director, MRC Cancer Unit, co-lead for the CRUK Cambridge Centre Early Detection Programme at the Hutchison-MRC Research Centre and Director of Medical Studies for Trinity College Cambridge.
Read more about how Cambridge is working to cure cancer through early detection and precision medicine.