This idea must die: We can’t find new antimicrobials fast enough to make a difference
Dr Anna-Maria Pappa says her new technology will help win the battle against drug-resistant pathogens.
In the battle against infections, we face an enemy that never sleeps. The bacteria, parasites, viruses and fungi that attack our bodies are constantly evolving, and our overuse of antibiotics in human and veterinary medicine means dangerous pathogens are becoming resistant to our drugs. Indeed, the World Health Organization warns that, without urgent action, we’re heading for a post-antibiotic era – a time when common infectious diseases like pneumonia and tuberculosis will be impossible to treat.
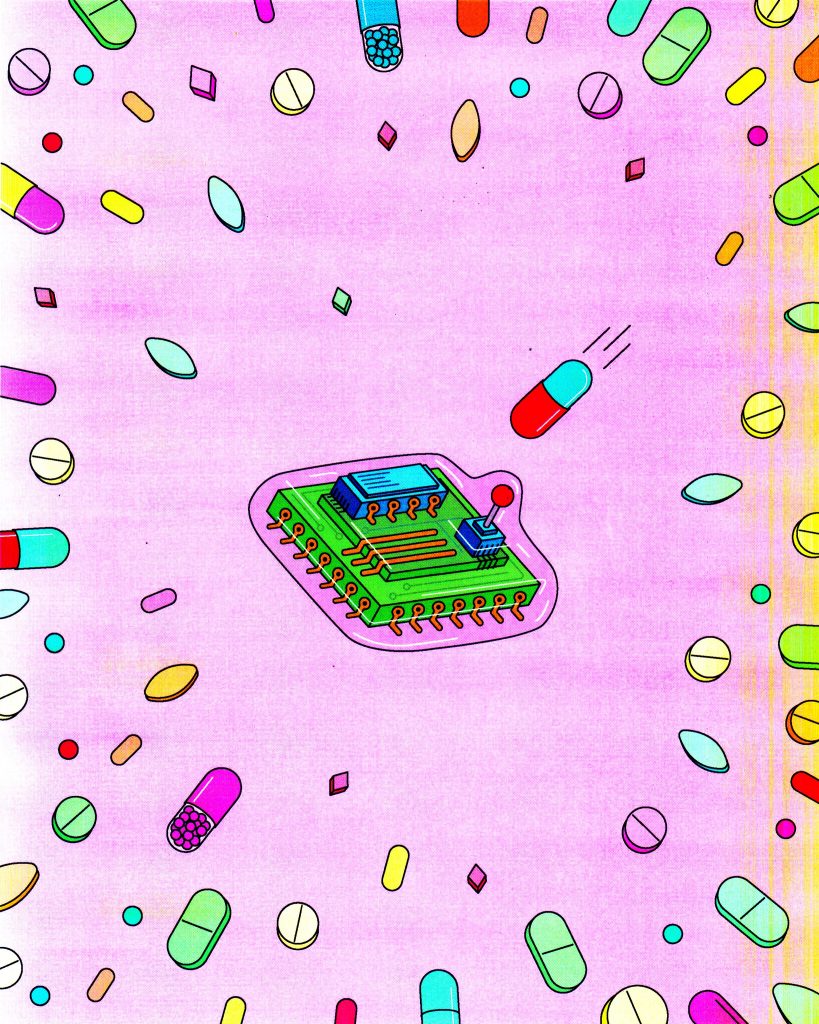
But new drugs that can attack pathogens in totally new ways do exist – it’s just that finding them is like looking for a needle in a haystack. That’s where my research comes in: together with synthetic biologists at Cornell and materials scientists at Stanford, I’m working on speeding up the hunt for novel classes of antimicrobials with a new technology: a minute piece of cell membrane grown on the surface of an electronic chip.
Living cells are bags of genetic information and biochemical machinery surrounded by a membrane. Cell membranes are amazing structures and they’re integral to cell homeostasis. Destroy the membrane of any cell – bacterial or mammalian – and it will die. That’s why cell membranes are targets for so many antimicrobial drugs.
Our simple membrane-chip sandwich is so small, you can have multiple arrays capable of testing many drugs at the same time. It can be used anywhere, not just in a lab – even at the point of care
When we form a bacterial membrane on top of the electronic device it creates a barrier that affects the electronic signal. The device cannot operate normally with this barrier, so if we add a drug that destabilises or destroys the membrane, it changes the signal. This gives us quantitative information on the destructiveness of different concentrations of a compound.
Compared with using whole-cell cultures for testing or screening drugs, our technology is more sensitive and reliable, as well as being more robust and scalable. Culturing cells for whole-cell assays isn’t easy, and you need strictly controlled environmental conditions. Our device can be used anywhere and not just in a lab – even at the point of care. And our simple membrane-chip sandwich is so small that you can have multiple arrays capable of testing many drugs at the same time.
Our new technology has lots of exciting potential uses. We can use it to assess the potency of drugs that target cell membranes, and in drug discovery to screen thousands of compounds for drugs that work in novel ways. And because we can test mammalian cell membranes alongside microbial membranes, we can identify compounds that will kill microbes but are safe for humans.
We hope our technology can massively accelerate the drug discovery pipeline.
One big challenge in the field of antimicrobial resistance is the lack of new drugs, but we hope our technology can massively accelerate the drug discovery pipeline. Part of the problem is that we lack strategies to assess the potency of millions of compounds; being able to develop hundreds of compounds is only part of the solution. You also need technologies that can identify them quickly. It’s not that we lack antimicrobials, it’s just the process of finding them is really time consuming, but we hope we have a solution.
For example, there’s a promising class of drug called antimicrobial peptides that work by destroying cell membranes, and which our collaborators are making in the lab. If you take two similar peptides with just one difference in their chemical backbone, only one of which is capable of killing bacteria, our technology is able to find it.
Beyond antimicrobial resistance, the technology can help us understand how cells interact with their environment. That’s really useful in studying how viruses infect human cells, because it tells us which ‘lock and key’ a virus uses to enter – and replicate in – a host cell.
At the moment, we’re working towards a prototype device that can be mass-produced. In future, we hope that the technology could also be used in precision medicine. For example, we could take bacteria from a patient with sepsis, turn that into a bespoke membrane-on-chip device, and use it to select the best drug to treat the patient, the drug that’s most potent against their bacteria but least harmful to their own cells. So, far from running out of options to combat dangerous pathogens, we might just be tipping the scales back in our favour.
Dr Anna-Maria Pappa took up the Maudslay-Butler Research Fellowship at Pembroke College. She also holds an Oppenheimer Research Fellowship.